US
US
New York
NY
10019
USA
Transforming Healthcare
The Peterson Center on Healthcare accelerates the adoption of innovative solutions that improve quality and lower cost on a national scale.
Read More
Evaluating Digital Health Technologies
The Peterson Health Technology Institute provides independent evaluations of innovative healthcare technologies to improve health and lower costs.
Read More
Addressing Unsustainable Healthcare Costs
We are supporting efforts to set and track healthcare spending targets at the state level.
Read More
Building Evidence for Action
To improve healthcare quality in the U.S., we must first understand how our system is performing.
Read More
Addressing Shortages and High Prices of Life-Saving Medications
To address risks posed to patients from chronic shortages and rising prices of life-saving generics, we support Civica Rx, a not-for-profit generic drug company.
Read MoreHealthcare Challenges
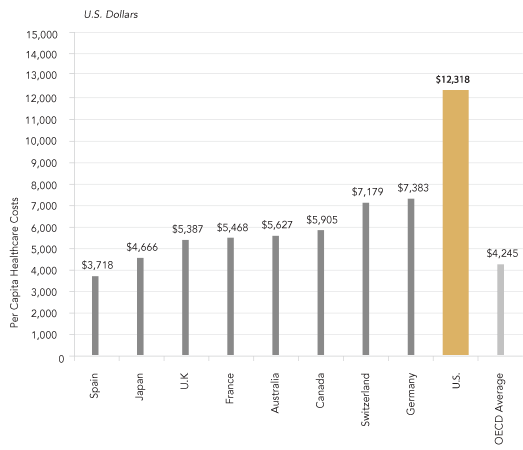
The U.S. healthcare system is the most expensive in the world, and our costs are projected to grow dramatically in the coming years. Yet, our health outcomes are worse than many other nations. Ineffective care puts our population through unnecessary treatments, leaves us in poorer health, and shortens our life expectancy. The high cost of healthcare makes everything in our economy more expensive, and reduces the resources that individual families and the nation have to invest in our collective future.
Read More SHARE
Strategies for Change
The Peterson Center on Healthcare is dedicated to transforming U.S. healthcare into a high-performance system by improving quality and lowering cost. Our programs are designed to accelerate improvement by:
- Finding and validating innovative solutions,
- Facilitating their broad adoption, and
- Fostering the conditions to improve healthcare nationally.
Read More SHARE
Our Initiatives
The Peterson Center on Healthcare collaborates with key thought leaders and stakeholders across the healthcare system, including health providers, consumer advocacy groups, health insurance plans, and major purchasers such as employers, states, and unions. Our grant-making, partnerships, and research are focused on scaling innovative solutions that improve quality and lower costs on a national scale.
Read More SHARE
About Us
The Peterson Center on Healthcare is a non-profit organization dedicated to making higher quality, more affordable healthcare a reality for all Americans. The organization is working to transform U.S. healthcare into a high-performance system by finding innovative solutions that improve quality and lower costs, and accelerating their adoption on a national scale. Established by the Peter G. Peterson Foundation, the Center collaborates with stakeholders across the healthcare system and engages in grant-making, partnerships, and research.
Read More SHARENEWS AND VIEWS From the Field
Latest from the Peterson Center on Healthcare
Latest from Our Partners


Updates from Around the Nation

SOURCE: POLITICO Future Pulse

SOURCE: Philanthropy News Digest

SOURCE: Fierce Healthcare

SOURCE: HIT Consultant

SOURCE: Healthcare Innovation


SOURCE: RevCycleIntelligence

SOURCE: KFF Health News

SOURCE: Becker's Hospital Review