Evolving Remote Monitoring: An Evidence-Based Approach to Coverage and Payment
Last Updated April 16, 2025
Increasingly, patients, including many Medicare beneficiaries, are tracking their vital signs and other health data with wearables and connected devices that transmit information back to their doctor or care team. Providers can use that data to monitor patients’ health and adjust their medications and care plans.
Unfortunately, in many fee-for-service environments, provider payments for these services are not linked to outcomes. In fact, in Medicare, payments for these remote monitoring services are the same across conditions and can continue indefinitely—regardless of whether they generate clinical benefits for the patient.
Now is the time for payers and policymakers to:
- Align coverage and reimbursement for remote monitoring services to clinical value
- Ensure access to high-impact remote monitoring services, and
- Improve data collection of remote monitoring services.
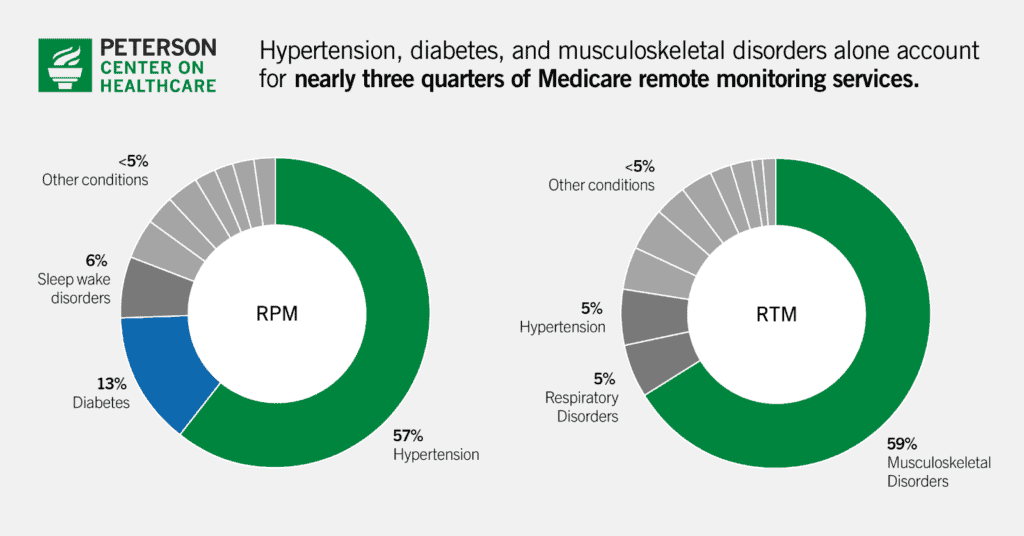
This report synthesizes three PHTI evaluations of digital tools to treat diabetes, hypertension, and musculoskeletal disorders, covering the conditions associated with the majority of spending and utilization for remote monitoring services. In 2023, diabetes and hypertension monitoring represented 73% of total RPM spending in traditional Medicare. Musculoskeletal disorder monitoring was the most common application for RTM, representing 59% of all RTM episodes and almost half of RTM spending.
While remote monitoring solutions are currently used by only a subset of people enrolled in Medicare, their use—and duration of use—is growing rapidly. Moreover, the sector is being flooded with an array of new products from hundreds of technology companies marketing the potential to increase provider revenue for longer periods of time. Medicare currently has no limit on duration of billing for remote monitoring, which means providers are reimbursed up to $1,110 per patient, year after year. The report comes at a pivotal moment for remote monitoring technology, given the importance of finding valuable technologies to better treat patients while preventing a rapid increase in spending on ineffective and wasteful care.
Download the Report
Evolving Remote Monitoring: An Evidence-Based Approach to Coverage and Payment
Policy in Action: Advancing Healthcare Affordability Through Strategic Engagement
In this letter, the Center’s Executive Director Caroline Pearson outlines recent policy engagements to advance healthcare affordability.
Center Responds to CMS Proposed Rule on Hospital Outpatient Prospective Payment System
The Center offers recommendations to strengthen hospital price transparency, advance site-neutral payment policy, and improve Medicare Advantage data reporting.
Center Responds to CMS Proposed Rule on Medicare Physician Fee Schedule
The Center offers recommendations to align Medicare payments with clinical value, advance digital mental health treatment, and promote high-value digital health tools.


